
2025 STI Awareness Week

Join communities across Georgia for STI Awareness Week, April 13–19, 2025.
This national observance is a vital opportunity to raise awareness about sexually transmitted infections (STIs), reduce stigma, and empower individuals with the tools to Talk. Test. Treat.
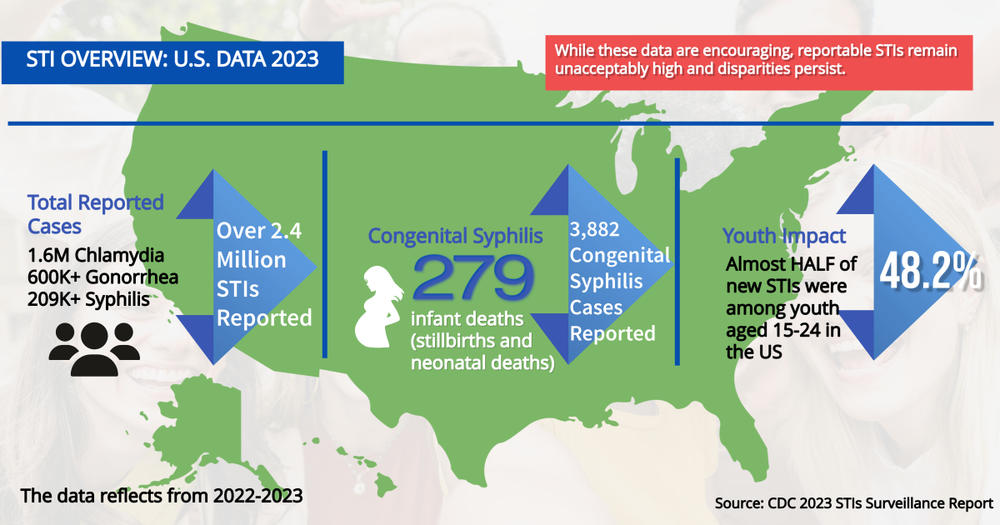
In 2023, more than 2.4 million STIs were reported in the U.S., including over 1.6 million chlamydia, 600,000 gonorrhea, and 209,000 syphilis cases.
🔺 Nearly 4,000 cases of congenital syphilis were also reported, including 279 infant deaths—a tragic but preventable outcome.
📊 Almost half of all reported cases occurred in people aged 15–24.
📈 Certain communities continue to experience higher infection rates, underscoring the ongoing need for access to testing, education, and care.
In Georgia, STI rates mirror national trends and remain a significant public health concern, especially among young adults. But with the right tools, we can change the narrative. By staying informed, getting tested, and seeking timely treatment, we each have the power to protect our health and build a healthier Georgia.
Talk. Test. Treat. Protect: Prevention Starts with You
Prevention is a core focus of the Talk. Test. Treat. campaign. In addition to regular testing and timely treatment, using condoms consistently and correctly remains one of the most effective ways to reduce the risk of many STIs, including HIV.
To support prevention, Georgia offers free condoms through local health departments and confidential mail-order programs. These resources help reduce barriers and empower individuals to take control of their sexual health.
Take action today—Talk. Test. Treat.
Protect yourself, your partner, and your community.
🔗 Find free condoms near you: Click Here

Georgians
If you are sexually active, or thinking of becoming sexually active, you must Talk. Test. Treat. to protect your health. These three small actions can have a significant impact on your sexual health!
-
Talk
Talk openly and honestly to your partner(s) and your healthcare provider about sexual health and sexually transmitted infections, or STIs.
Talk with your partner(s) BEFORE having sex. Not sure how? We have tips to help you start the conversation. Make sure your discussion covers several important ways to make sex safer:
- Talk about when you were last tested and suggest getting tested together.
- If you have an STI (like herpes or HIV), tell your partner.
- Agree to only have sex with each other.
- Use condoms the right way for every act of vaginal, anal, and oral sex throughout the entire sex act (from start to finish).
Talk with your healthcare provider about your sex life as it relates to your health. This helps your healthcare provider understand what STI tests you should get and how often.
Here are a few questions you should expect and be prepared to answer honestly:
- Have you been sexually active in the last year?
- Do you have sex with men, women, or both?
- In the past 12 months, how many sexual partners have you had?
- Do you have anal, oral, or vaginal sex?
- What are you doing to protect yourself from infection?
Not all medical checkups include STI testing, so don’t assume that you’ve been tested unless you discuss it with your provider. If your provider does not discuss sex or STI testing with you, bring it up.
Ask your healthcare provider whether certain vaccines, such as the hepatitis B vaccine or the HPV vaccine, are right for you.
-
Test
Get tested. It’s the only way to know for sure if you have an STI.
Many STIs don’t cause any symptoms, so you could have one and not know. If you’re having sex, getting tested is one of the most important things you can do to protect your health.
Learn which tests the CDC recommends for you. Even if you’re pregnant, you can still get an STI. If you’re having sex, you’re still at risk.
Find out what STI care options are available near you. In addition to traditional, in-person visits, other options that may be available include:
- Video or phone appointments with your healthcare provider.
- Express visits allow walk-in STI testing and treatment appointments without a complete clinical exam.
- Pharmacies and retail clinics, such as grocery stores or big-box stores, offer on-site testing and treatment.
- At-home collection, where you collect your own sample and take or mail it to a lab for testing.
If you’re not comfortable talking with your regular healthcare provider about STIs, find a clinic near you that offers confidential testing that is free or low-cost.
-
Treat
If you test positive for an STI, work with your healthcare provider to get the correct treatment.
Some STIs can be cured with the right medicine, and all STIs are treatable. Make sure your treatment works by doing these things:
- Take all of the medication your healthcare provider prescribes, even if you start feeling better or your symptoms go away.
- Don’t share your medicine with anyone.
- Avoid having sex again until you and your sex partner(s) have all completed treatment.
Your healthcare provider can talk with you about which medications are right for you.

Providers
While the idea of Talk. Test. Treat. is simple, STI prevention and treatment are not one-size-fits-all. We encourage you, our Georgia healthcare providers, to revisit the many ways that you can empower your patients to take charge of their sexual health.
-
Talk
Providing the best medical care possible means talking to your patients about sexual health.
Taking a sexual history should be a part of routine care.
Talking about sexual health can be challenging, but studies show that patients want to be asked about sex. The following tips can help to ensure the most productive conversations with your patients:
- Create a welcoming and inclusive clinic or office environment to help foster trust with your patients before their visit even starts. For example, you can use these tips to make your office teen-friendly.
- Make sure your patients are comfortable and in a private space, especially before asking sensitive questions; this includes assuring patients that everyone in your office is protecting their confidentiality.
- Help normalize sexual health questions and STI/HIV testing recommendations by letting your patients know you ask these questions and offer these services to all patients, as sexual health is a regular part of a person’s overall health and well-being.
- Avoid making assumptions about your patients; asking is the only way to know for sure. Standardize sexual orientation/gender identity (SOGI) questions and use open-ended questions when taking a sexual history.
- If your patient is hesitant to answer a question, try rephrasing it or briefly explaining why you are asking it.
- Ensure you and your patient understand the terms used to avoid confusion.
Counsel your patients on safer sex, and ensure that they know about today’s many prevention options. With condoms, hepatitis B and HPV vaccines, and even a daily medication to prevent HIV infection, there have never been more ways for your patients to protect themselves.
Specific STI diagnoses can cause fear and anxiety in your patient.
Use CDC counseling messages in the 2021 STI Treatment Guidelines to help alleviate these concerns.
-
Test
Test your patients for STIs as recommended.
Use the sexual history to determine which STIs you should test for and the anatomical sites to test.
STI screening recommendations for different patient populations are available. Below is a brief overview.
- All adults and adolescents between the ages of 13 and 64 should be tested at least once for HIV.
- All sexually active women younger than 25 years should be tested for gonorrhea and chlamydia every year. Women 25 years and older with risk factors such as new or multiple sex partners or a sex partner who has an STI should also be tested for gonorrhea and chlamydia every year.
- Everyone who is pregnant should be tested for syphilis, HIV, hepatitis B, and hepatitis C starting early in pregnancy. Those at risk for infection should also be tested for chlamydia and gonorrhea starting early in pregnancy. Repeat testing may be needed in some cases.
- All sexually active gay, bisexual, and other men who have sex with men should be tested:
- At least once a year for syphilis, chlamydia, and gonorrhea. Those with multiple or anonymous partners should be tested more frequently (e.g., every 3 to 6 months).
- At least once a year for HIV and may benefit from more frequent HIV testing (e.g., every 3 to 6 months).
- At least once a year for hepatitis C, if living with HIV.
- Anyone who engages in sexual behaviors that could place them at risk for infection or shares injection drug equipment should get tested for HIV at least once a year.
Remember that screening recommendations are sources of clinical guidance, not prescriptive standards. Always consider a patient’s sexual history and the burden of disease in their community.
Once a patient has been tested, make sure they know how they will get their test results.
-
Treat
Follow CDC’s STI Treatment Guidelines to ensure appropriate treatment and care.
The 2021 STI Treatment Guidelines are the most current recommendations for treating patients with or at risk of infection.
Important treatment topics to be aware of:
Expedited Partner Therapy (EPT) may be an option in cases where a patient’s partner is unwilling or unable to access care.
- Learn about EPT on the CDC’s website or contact your state or territorial health department for jurisdiction-specific information.
Reinfection is common for some STIs. Encourage your patients to return for follow-up testing in three months.
Drug-resistant gonorrhea is an immediate public health threat requiring urgent and aggressive action.
Preserve our last treatment option by only treating your patients with the recommended treatment (ceftriaxone 500mg intramuscularly in a single dose).