
DPH Home Visiting Program

Stronger Together - Partnering to Support Your Patients Beyond the Office.
The DPH Home Visiting Program provides services by public health department nurses and trained staff, to expectant mothers from pregnancy until the first year of their baby's life, at no cost to patients or providers. The program focuses on assisting pregnant women with high-risk conditions or risk factors that increase the likelihood of poor pregnancy outcomes. Although enrollment can occur after delivery, early intervention is preferred.
DPH home visitors can provide monitoring and services to detect potential warning signs, complications, and problems between provider appointments. Early detection increases the likelihood of prompt intervention and referrals for further assessment and treatment.
Monitoring and Service Components:
-
Maternal (Pregnancy and Postpartum)
Clinical assessment for pregnancy and postpartum complications including:
- Blood pressure assessment
- Fingerstick for blood glucose (if indicated)
- Weight
- Urine dipstick
- Fetal Heart Tones
Screening for pregnancy and postpartum warning signs and symptoms:
- Vaginal bleeding or fluid leaking during pregnancy
- Vaginal bleeding or discharge after pregnancy
- Severe Headaches
- Severe abdominal pain
- Extreme swelling of hands or face
- Changes in vision
- Severe swelling, redness, or pain in the leg or arm
- Trouble breathing
- Chest pain or fast-beating heart
- Depression and anxiety
-
Infant (Nutrition and Development)
Clinical assessment includes:
- Feeding
- Weight
- Head circumference
- Developmental screening
What Providers Should Do
Healthcare providers should refer...
-
Maternal patients with
- Hypertension or Gestational Hypertension
- Preeclampsia
- Diabetes
- Multiple gestations
- Prior preterm delivery
- Preterm labor
- Chronic conditions or co-morbidities
- Prior 2nd-trimester pregnancy loss
- Prior fetal/neonatal death
- Pre-existing health conditions
- Substance use disorder
- Mental health condition
- Poor support system
- Difficulty complying with provider recommendations and/or follow-up (e.g., keeping appointments)
- Other medical conditions or concerns for poor outcomes
-
Infant patients with
- Recent NICU discharge
- VLBW or LBW
- <36 weeks gestation at delivery
- Positive maternal screening for substances at delivery
- Suspected or confirmed congenital syphilis or HIV infection
- Poor maternal support system or other environmental concerns
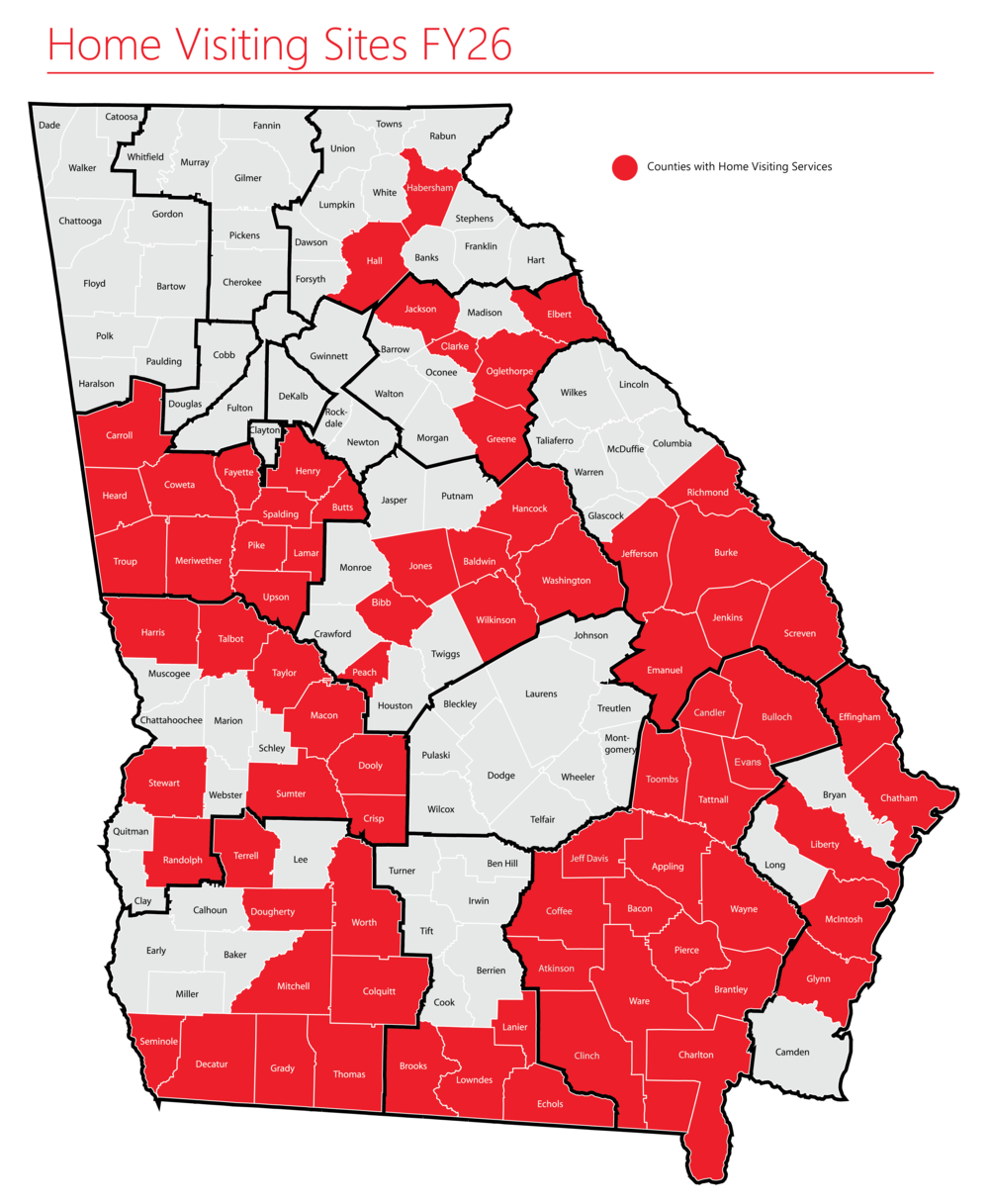
DPH Home Visiting Health District Sites
North Health District (Gainesville)
- Counties (Habersham and Hall)
Southeast Health District (Waycross)
- Counties (Appling, Atkinson, Bacon, Brantley, Bulloch, Candler, Charlton, Clinch, Coffee, Evans, Jeff Davis, Pierce, Tattnall, Toombs, Ware and Wayne)
East Central Health District (Augusta)
- Counties (Richmond, Jefferson, Emanuel, Burke, Screven, and Jenkins)
Coastal Health District (Savannah)
- Counties (Effingham, Liberty, Glynn, Chatham, and McIntosh)
District 4 Health District (LaGrange)
- Counties (Carroll, Heard, Coweta, Troup, Spalding, Meriwether, Upson, Butts, Pike, Fayette, Henry, and Lamar)
South Health District (Valdosta)
- Counties (Lowndes, Echols, Brooks and Lanier)
Northeast Health District (Athens)
- Counties (Clarke, Elbert, Greene, Jackson, Oglethorpe)
Southwest Health District (Albany)
- Counties (Terrell, Worth, Dougherty, Colquitt, Mitchell, Grady, Seminole, Decatur, and Thomas)
North Central Health District (Macon)
- Counties (Peach, Bibb, Jones, Baldwin, Wilkinson, Hancock, and Washington)
West Central Health District (Columbus)
- Counties (Harris, Talbot, Taylor, Macon, Dooly, Crisp, Sumter, Stewart, and Randolph)
Page updated 11/4/2025